Risk and opportunity management within SANBS
SANBS embraces risk as an essential enabler for setting and achieving its strategic objectives and purpose of being ‘Trusted to Save Lives’
![]() Risk Governance
Risk Governance
How SANBS manages risk and opportunity
SANBS has established risk management as an integral component of business processes.
Risk management is governed by an Enterprise Risk Management (ERM) Framework which provides a solid foundation to guide the organisation in embedding structured risk management processes to deliver sustained value.
Through the ERM process, risks and opportunities, which could affect the achievement of our iHEALTh strategy, are identified and managed within defined risk appetite and tolerance levels set by the Board. Management decisions to tolerate, treat, terminate or share risks and opportunities are taken based on these parameters.
As an essential health service provider of blood products and services, it is prudent that SANBS protects its donors and stakeholders from the potential adverse effects of risk and has therefore adopted a conservative risk approach.
SANBS follows an iterative and dynamic risk management process to ensure ongoing identification and evaluation of risks and opportunities in response to a continually evolving and rapidly changing internal and external environment. Risks and opportunities are also identified through stakeholder engagement.
Oversight of risk management is the responsibility of the Risk, Technology and Information Governance Committee. See our RTIG Committee.
Notable for 2021
Our material matters are reflected in our key risks and opportunities and represent the issues that have the most impact on our ability to create sustainable value for our stakeholders and influence our business model. Read more about our Material Matters page.
Of significance, as reported during the previous reporting period and until the date of this report, is the management of the risks associated with the Covid-19 pandemic, as well as the management of the impact on blood supply during the recent unrest in KZN.
Risk management continued to play a major role to ensure continuity of operations in response to these events by:
See focus of Risk, Technology and Information Governance Committee on the link and details of Risk and Opportunity Management below:
Managing our risks and opportunities to ensure we manage what matters most
BENEFITS DERIVED FROM PRACTISING GOOD RISK MANAGEMENT
NAVIGATING THROUGH A YEAR OF CRISIS AND CONFIDENTLY PAVING THE WAY INTO THE FUTURE
Our ERM framework is premised on global practical risk management practices including ISO31000 and King IVTM, and includes the identification, analysis, evaluation, treatment and monitoring of risks and opportunities from a position where we understand the context of our internal and external business environment and impact on our iHEALTh strategy.
Figure 1, demonstrates how the effort is driven by the Board, senior and middle management to manage and report on risks.

Figure 1

Figure 2: Risk management and risk reporting process
In addition, all lines of assurance are included (» See link), as part of the Board Committee oversight to ensure that roles, responsibilities and accountabilities for risk are clearly defined. See Figure 2.
CURRENT AND ONGOING FOCUS AREAS
Pre-empting and managing impacts caused by the Covid-19 pandemic
Two external events that initiated additional risk identification included:
Implementation of iHEALTh
Blood establishment computer system project management
SANBS RISK PROFILE (RISK HEATMAP OF TOP RISKS)
The residual risk level of strategy level risks currently identified and managed is depicted in the heatmap below:
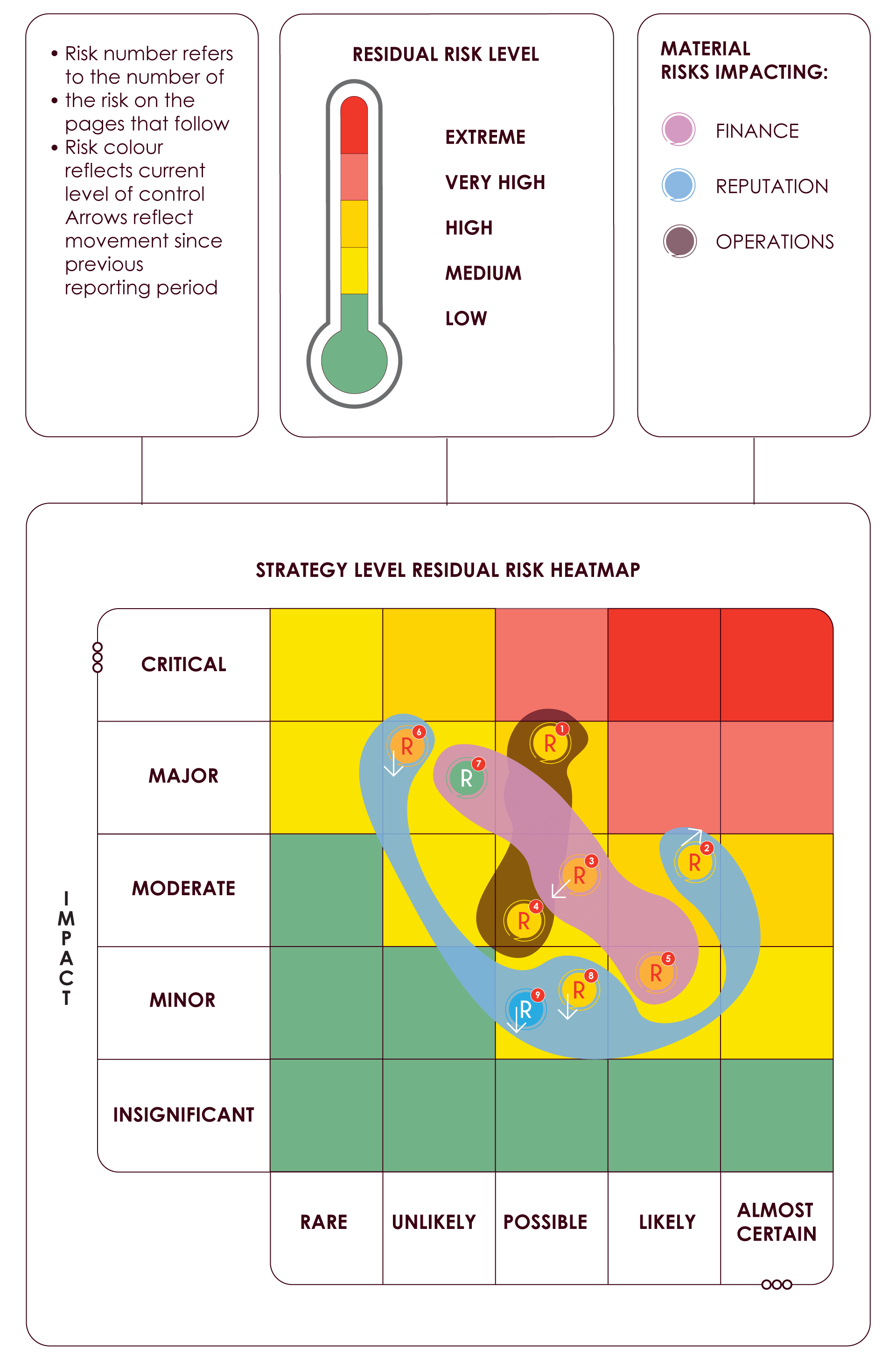
Likelihood
RISK PROFILE TREND
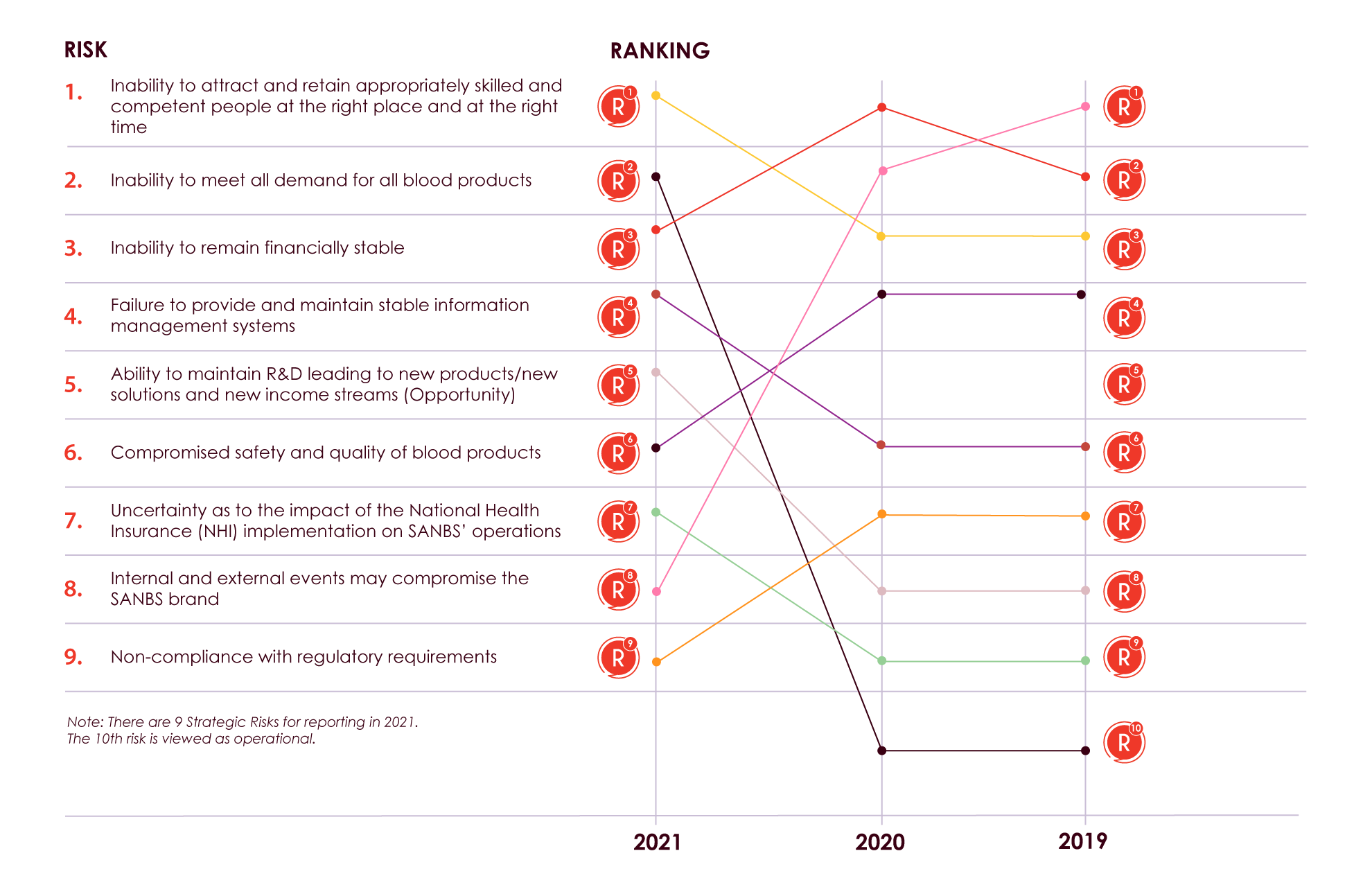
FY2021 TOP RISKS
| STRATEGY LEVEL RISK/OPPORTUNITY | KEY CAUSES, CONTROLS AND RISK TREATMENTS | |||||
|---|---|---|---|---|---|---|
| Year-on-year fluctuation | Increase | Decrease | Same | New | ||
Risk |
Key Causes |
Key Controls |
||||
|
Inability to attract and retain appropriately skilled and competent people at the right place and at the right time
iHEALThCapital |
||||||
Key risk treatment actions |
||||||
Covid-19 impact |
||||||

|
||||||
| STRATEGY LEVEL RISK/OPPORTUNITY | KEY CAUSES, CONTROLS AND RISK TREATMENTS | |||||
|---|---|---|---|---|---|---|
| Year-on-year fluctuation | Increase | Decrease | Same | New | ||
Risk |
Key Causes |
Key Controls |
||||
|
Inability to meet all demand for all blood products
iHEALThCapital |
||||||
Key risk treatment actions |
||||||
Covid-19 impact |
||||||

|
||||||
| STRATEGY LEVEL RISK/OPPORTUNITY | KEY CAUSES, CONTROLS AND RISK TREATMENTS | |||||
|---|---|---|---|---|---|---|
| Year-on-year fluctuation | Increase | Decrease | Same | New | ||
Risk |
Key Causes |
Key Controls |
||||
|
Inability to remain financially sustainable
iHEALThCapital |
||||||
Key risk treatment actions |
||||||
Covid-19 impact |
||||||

|
||||||
| STRATEGY LEVEL RISK/OPPORTUNITY | KEY CAUSES, CONTROLS AND RISK TREATMENTS | |||||
|---|---|---|---|---|---|---|
| Year-on-year fluctuation | Increase | Decrease | Same | New | ||
Risk |
Key Causes |
Key Controls |
||||
|
Failure to provide and maintain stable information management systems
iHEALThCapital |
||||||
Key risk treatment actions |
||||||
Covid-19 impact |
||||||

|
||||||
| STRATEGY LEVEL RISK/OPPORTUNITY | KEY CAUSES, CONTROLS AND RISK TREATMENTS | |||||
|---|---|---|---|---|---|---|
| Year-on-year fluctuation | Increase | Decrease | Same | New | ||
Risk |
Key Causes |
Key Controls |
||||
|
Ability to maintain R&D leading to new products/new solutions and new income streams (Opportunity)
iHEALThCapital |
||||||
Key risk treatment actions |
||||||
Covid-19 impact |
||||||

|
||||||
| STRATEGY LEVEL RISK/OPPORTUNITY | KEY CAUSES, CONTROLS AND RISK TREATMENTS | |||||
|---|---|---|---|---|---|---|
| Year-on-year fluctuation | Increase | Decrease | Same | New | ||
Risk |
Key Causes |
Key Controls |
||||
|
Compromised safety and quality of blood products
iHEALThCapital |
||||||
To note: Currently there is no proof that Covid-19 is transfusable |
||||||
Key risk treatment actions |
||||||
Covid-19 impact |
||||||

|
||||||
| STRATEGY LEVEL RISK/OPPORTUNITY | KEY CAUSES, CONTROLS AND RISK TREATMENTS | |||||
|---|---|---|---|---|---|---|
| Year-on-year fluctuation | Increase | Decrease | Same | New | ||
Risk |
Key Causes |
Key Controls |
||||
|
Uncertainty as to the impact of the National Health Insurance (NHI) implementation on SANBS operations
iHEALThCapital |
||||||
Key risk treatment actions |
||||||
Covid-19 impact |
||||||

|
||||||
| STRATEGY LEVEL RISK/OPPORTUNITY | KEY CAUSES, CONTROLS AND RISK TREATMENTS | |||||
|---|---|---|---|---|---|---|
| Year-on-year fluctuation | Increase | Decrease | Same | New | ||
Risk |
Key Causes |
Key Controls |
||||
|
Internal and external events may compromise the SANBS brand
iHEALThCapital |
||||||
Key risk treatment actions |
||||||
Covid-19 impact |
||||||

|
||||||
| STRATEGY LEVEL RISK/OPPORTUNITY | KEY CAUSES, CONTROLS AND RISK TREATMENTS | |||||
|---|---|---|---|---|---|---|
| Year-on-year fluctuation | Increase | Decrease | Same | New | ||
Risk |
Key Causes |
Key Controls |
||||
|
Non-compliance with regulatory requirements
|
||||||
Key risk treatment actions |
||||||
Covid-19 impact |
||||||

|
||||||

